COVID-19 Trackers
입력 2020.10.09 (14:57)
수정 2020.10.09 (16:45)
읽어주기 기능은 크롬기반의
브라우저에서만 사용하실 수 있습니다.
[Pkg]
Twenty-two COVID-19 cases were confirmed in a building in Seoul on March 8. Epidemiological investigators were the first to be dispatched to the scene.
[Soundbite]
Kim Mi (Epidemiologist): All of a sudden, there were seven to eight media reports daily. I was taken aback. The surveillance camera footage of the freight elevator showed that most people inside it weren’t wearing masks. We concluded it was a critical situation. We ordered the shutdown of the eleventh floor, where the call center is located. We set up a screening station on the first floor and began to test people aggressively.
Some 16-thousand people in the vicinity received an emergency text message. Thanks to a swift investigation that traced the source of infections and close contacts, epidemiologists were able to stop the spread.
We met with the epidemiologist who was at the front line of the COVID-19 response at the time.
[Soundbite]
Jang Han-aram (Epidemiologist): It was the first cluster infection in the Seoul metropolitan area. Obtaining the list of people who were in the building and their contacts, and placing them under self-quarantine quickly made it possible to stop the spread of the virus. I think the epidemiological investigation was deeply meaningful.
A new case was confirmed at dawn. First, the infected persons’ movements are traced through their testimonies.
[Soundbite]
Kim Seong-gon (Epidemiologist): Did you stay home on September 6, 7, and 8?
[Soundbite]
Park Dae-gyu (Epidemiologist): Do any of the employees have a fever or respiratory symptoms? You met with three people?
The whiteboard is filled with information on infections.
[Soundbite]
Jang Han-aram (Epidemiologist): They must have visited a nursing home on August 30 and in early September. I think we’ll have to look into that. Trace their movements before September 3. Get a list of people and start contacting them. Then classify the contacts right away.
While the investigators trace the transmission and identify close contacts, epidemiologists visit the site of the outbreak.
[Soundbite]
Why are you going there?
[Soundbite]
Jang Han-aram (Epidemiologist): There are 2 infected patients at a nursing home. They contracted the virus through different routes. I’m going to find out if those two cases are related. We have to find out the patients’ movements within the hospital, the time of their hospitalization and discharge, and their contacts and transmission routes. We must also assess the risk to decide what measures to take regarding the facility, patients and the staff. That’s why I’m going there.
[Soundbite]
How many epidemiologists are there in your team?
[Soundbite]
Jang Han-aram (Epidemiologist): We had 6 before. But as cases spiked in the capital area, we have 12 now. 4 epidemiologists work every day. We can forecast the number of cases in Incheon. We thought 4 epidemiologists a day could handle that number, so we recruited 6 more people.
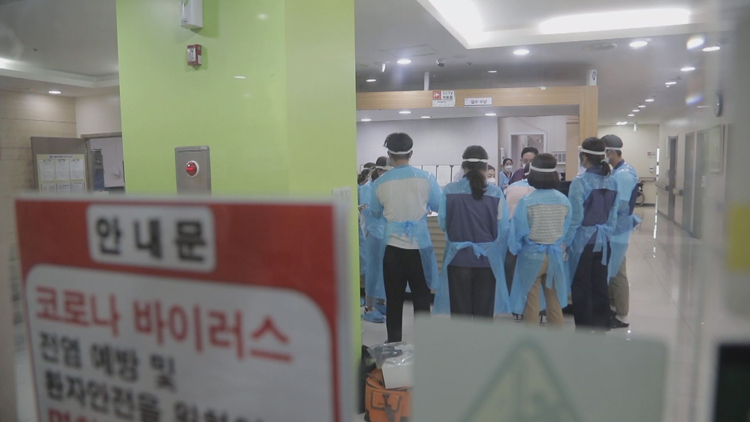
This is the nursing home where patients have tested positive for COVID-19. Fast response is critical to mitigating the spread of COVID-19.
[Soundbite]
I should take a picture of this.
[Soundbite]
Kim Seong-gon (Epidemiologist): The nursing home will likely be placed under quarantine. Because it’s a hospital and a high-risk facility, it could be locked down if there are too many infected people and close contacts.
The most critical time is two days before a patient develops first symptoms and right before they are admitted to a hospital. It’s the most infectious period. Prior to an investigation, it’s essential to put on a protective suit, a mask and gloves.
[Soundbite]
Jang Han-aram (Epidemiologist): Check the list of patients, and identify employees who are currently working and patients who were discharged between August 25 and September 9. And the two of you go check surveillance camera footage. Start with the patient who was admitted on August 25.
That day, the epidemiologists managed to prevent additional spread by surveying around 800 people - doctors, patients, vendors and visitors who crossed paths with the infected. We were no longer allowed to continue filming due to transmission concerns.
[Soundbite]
Have you had dinner?
[Soundbite]
Jang Han-aram (Epidemiologist): I grabbed a bite near the hospital after finishing the investigation. I had no time to have lunch. The investigation ended at 5 p.m. Epidemiologists have to work in gowns, face shields, and gloves. Once you’re in, it’s hard to take a break. It’s a hassle to get changed, so once we start, we don’t have meals until we finish.
Epidemiologists of Incheon City work in teams of four, rotating in three shifts around the clock.
[Soundbite]
Jang Han-aram (Epidemiologist): People who visit places where an infected person was at the same time are classified as “contacts.” Classifying and tracing contacts is the purpose of epidemiological studies. We identify contacts, test them and place them under quarantine. Contacts of COVID-19 cases can develop symptoms and become infectious any time. We quarantine them in advance to prevent transmission.
[Soundbite]
In the first stage, we find out when an infected person first developed symptoms. We trace their movements and contacts from two days before that time. Then, we wait for the GPS data. Once we receive it, we check with the patient to reconfirm the route. We do this to identify contacts once again (based on the GPS data).
[Soundbite]
Infected persons do not know who they came across when they visited a public facility. In that case, epidemiologists contact a public health center in the region that the infected person visited, and visit the area to check surveillance camera footage. They ask the health center to identify contacts and conduct tests along with active monitoring.
Back in May, a cluster outbreak occurred at a nightclub in Itaewon. A private academy instructor who was at the club that night lied about his itinerary, but the truth was revealed through an epidemiological study.
[Soundbite]
The GPS data is completely different from the patient’s testimony. He visited the Hongik University area and said he was unemployed, but his friends say he has a job. From the GPS data it’s clear he works near a supermarket.
[Soundbite]
Jang Han-aram (Epidemiologist): It was very frustrating, and dangerous, too. When the academy instructor tested positive, he was highly infectious, but his close contacts slipped through the net. It was a grave situation, so we took immediate action.
[Soundbite]
An Incheon academy instructor who had visited an Itaewon nightclub has caused a septenary infection. The instructor’s student, customers of a singing room, guests at a birthday party, and restaurant customers have contracted the virus. The virus also spread to another restaurant, infecting another customer and family members.
Because of the instructor’s false testimony, his students also became infected.
[Soundbite]
(Patient of secondary transmission): All because of that single lie...I wondered why he had to lie.
One hundred and 25 schools were closed. When infected people lie, the consequences can be quite serious. Encouraging them to tell the truth is critical.
[Soundbite]
Jang Han-aram (Epidemiologist): Hello. I’m an epidemiologist at Incheon City. I can’t remember everything. Please say what you remember. I’m here to help you go through what you can remember.
[Soundbite]
(Infected person): There were a lot of places I visited...
[Soundbite]
Jang Han-aram (Epidemiologist): You’re sorry? You didn’t have any symptoms. How would you have known? You don’t need to be sorry. We’re grateful that you’ve been diagnosed so that we can prevent further infections.
Seasoned epidemiologists know how to make infected people feel at ease and convince them to cooperate.
[Soundbite]
Jang Han-aram (Epidemiologist): I think it is out of fear. They feel pressure to have their disease confirmed and their itinerary revealed. Many people still view COVID-19 patients in a negative light. They are afraid people will criticize them if their movements are disclosed. They end up hiding the truth because of the criticism.
[Soundbite]
(Worker at logistics center): When I asked what was going on, they told me a person was confirmed. I asked when and where but they said they couldn't say. That person worked at the packaging line on the 12th, I found out through the news that one of my co-workers had tested positive.
This woman contracted the virus even though she followed prevention rules. Her husband also ended up testing positive for COVID-19. If only the truth had been told, if only the critical time had not been lost, this family wouldn’t be in this distress.
[Soundbite]
Honey, wake up. Everyone else is up and all right. You’re the only one lying in bed. Your daughter and I are all here. Honey, can you hear me? Please, wake up.
[Soundbite]
Jang Han-aram (Epidemiologist): When patients are diagnosed with COVID-19, they must feel scared and frustrated. Cooperating with epidemiologists is the only way to protect themselves and people around them. We’re not trying to force information out of you. This is necessary to protect people you care about. Please, understand that.
[Soundbite]
(Epidemiologist at public health center): You cannot go into the hallway or use the elevator. Basically, you won’t be able to leave the room.
The average duration of a phone call with an infected patient is one hour. It’s intensive emotional labor.
[Soundbite]
Jang Han-aram (Epidemiologist): We’re seeing a new spike in COVID-19 cases. A growing number of people are refusing to cooperate with the investigators. In that case, epidemiologists have no choice but to bring up punishment or penalty. Some people even accuse the state of threatening and oppressing them. In extreme cases, they even slander my parents. It’s very discouraging. We conduct these investigations to protect infected patients and their loved ones. But they see me as an oppressor...
It’s been nine months since the COVID-19 pandemic began. Epidemiologists say they have hit a limit, both mentally and physically.
[Soundbite]
Park Eun-jeong (Epidemiologist at public health center): New cases occur randomly, day and night. I have to work until dawn, and I’m sleep-deprived.
The level of stress is hard to express in words.
[Soundbite]
Jang Han-aram (Epidemiologist): I started smoking after I began epidemiological investigations. I also drink a lot of coffee. This is how I relieve stress. Your faith and trust in people gets shattered. You become disappointed and even angry, and that’s how stress keeps building up.
According to a study, epidemiologists experienced the most frustration among jobs related to COVID-19. They were also found to experience above-average levels of mental exhaustion, reaching the state of burnout.
[Soundbite]
Jang Han-aram (Epidemiologist): I want to go camping. I want to set up a tent somewhere quiet and eat alone, enjoying the sound of a stream.
Epidemiologists are still battling COVID-19 on the front line. Even 24 hours a day is not enough to accomplish their task.
Twenty-two COVID-19 cases were confirmed in a building in Seoul on March 8. Epidemiological investigators were the first to be dispatched to the scene.
[Soundbite]
Kim Mi (Epidemiologist): All of a sudden, there were seven to eight media reports daily. I was taken aback. The surveillance camera footage of the freight elevator showed that most people inside it weren’t wearing masks. We concluded it was a critical situation. We ordered the shutdown of the eleventh floor, where the call center is located. We set up a screening station on the first floor and began to test people aggressively.
Some 16-thousand people in the vicinity received an emergency text message. Thanks to a swift investigation that traced the source of infections and close contacts, epidemiologists were able to stop the spread.
We met with the epidemiologist who was at the front line of the COVID-19 response at the time.
[Soundbite]
Jang Han-aram (Epidemiologist): It was the first cluster infection in the Seoul metropolitan area. Obtaining the list of people who were in the building and their contacts, and placing them under self-quarantine quickly made it possible to stop the spread of the virus. I think the epidemiological investigation was deeply meaningful.
A new case was confirmed at dawn. First, the infected persons’ movements are traced through their testimonies.
[Soundbite]
Kim Seong-gon (Epidemiologist): Did you stay home on September 6, 7, and 8?
[Soundbite]
Park Dae-gyu (Epidemiologist): Do any of the employees have a fever or respiratory symptoms? You met with three people?
The whiteboard is filled with information on infections.
[Soundbite]
Jang Han-aram (Epidemiologist): They must have visited a nursing home on August 30 and in early September. I think we’ll have to look into that. Trace their movements before September 3. Get a list of people and start contacting them. Then classify the contacts right away.
While the investigators trace the transmission and identify close contacts, epidemiologists visit the site of the outbreak.
[Soundbite]
Why are you going there?
[Soundbite]
Jang Han-aram (Epidemiologist): There are 2 infected patients at a nursing home. They contracted the virus through different routes. I’m going to find out if those two cases are related. We have to find out the patients’ movements within the hospital, the time of their hospitalization and discharge, and their contacts and transmission routes. We must also assess the risk to decide what measures to take regarding the facility, patients and the staff. That’s why I’m going there.
[Soundbite]
How many epidemiologists are there in your team?
[Soundbite]
Jang Han-aram (Epidemiologist): We had 6 before. But as cases spiked in the capital area, we have 12 now. 4 epidemiologists work every day. We can forecast the number of cases in Incheon. We thought 4 epidemiologists a day could handle that number, so we recruited 6 more people.
This is the nursing home where patients have tested positive for COVID-19. Fast response is critical to mitigating the spread of COVID-19.
[Soundbite]
I should take a picture of this.
[Soundbite]
Kim Seong-gon (Epidemiologist): The nursing home will likely be placed under quarantine. Because it’s a hospital and a high-risk facility, it could be locked down if there are too many infected people and close contacts.
The most critical time is two days before a patient develops first symptoms and right before they are admitted to a hospital. It’s the most infectious period. Prior to an investigation, it’s essential to put on a protective suit, a mask and gloves.
[Soundbite]
Jang Han-aram (Epidemiologist): Check the list of patients, and identify employees who are currently working and patients who were discharged between August 25 and September 9. And the two of you go check surveillance camera footage. Start with the patient who was admitted on August 25.
That day, the epidemiologists managed to prevent additional spread by surveying around 800 people - doctors, patients, vendors and visitors who crossed paths with the infected. We were no longer allowed to continue filming due to transmission concerns.
[Soundbite]
Have you had dinner?
[Soundbite]
Jang Han-aram (Epidemiologist): I grabbed a bite near the hospital after finishing the investigation. I had no time to have lunch. The investigation ended at 5 p.m. Epidemiologists have to work in gowns, face shields, and gloves. Once you’re in, it’s hard to take a break. It’s a hassle to get changed, so once we start, we don’t have meals until we finish.
Epidemiologists of Incheon City work in teams of four, rotating in three shifts around the clock.
[Soundbite]
Jang Han-aram (Epidemiologist): People who visit places where an infected person was at the same time are classified as “contacts.” Classifying and tracing contacts is the purpose of epidemiological studies. We identify contacts, test them and place them under quarantine. Contacts of COVID-19 cases can develop symptoms and become infectious any time. We quarantine them in advance to prevent transmission.
[Soundbite]
In the first stage, we find out when an infected person first developed symptoms. We trace their movements and contacts from two days before that time. Then, we wait for the GPS data. Once we receive it, we check with the patient to reconfirm the route. We do this to identify contacts once again (based on the GPS data).
[Soundbite]
Infected persons do not know who they came across when they visited a public facility. In that case, epidemiologists contact a public health center in the region that the infected person visited, and visit the area to check surveillance camera footage. They ask the health center to identify contacts and conduct tests along with active monitoring.
Back in May, a cluster outbreak occurred at a nightclub in Itaewon. A private academy instructor who was at the club that night lied about his itinerary, but the truth was revealed through an epidemiological study.
[Soundbite]
The GPS data is completely different from the patient’s testimony. He visited the Hongik University area and said he was unemployed, but his friends say he has a job. From the GPS data it’s clear he works near a supermarket.
[Soundbite]
Jang Han-aram (Epidemiologist): It was very frustrating, and dangerous, too. When the academy instructor tested positive, he was highly infectious, but his close contacts slipped through the net. It was a grave situation, so we took immediate action.
[Soundbite]
An Incheon academy instructor who had visited an Itaewon nightclub has caused a septenary infection. The instructor’s student, customers of a singing room, guests at a birthday party, and restaurant customers have contracted the virus. The virus also spread to another restaurant, infecting another customer and family members.
Because of the instructor’s false testimony, his students also became infected.
[Soundbite]
(Patient of secondary transmission): All because of that single lie...I wondered why he had to lie.
One hundred and 25 schools were closed. When infected people lie, the consequences can be quite serious. Encouraging them to tell the truth is critical.
[Soundbite]
Jang Han-aram (Epidemiologist): Hello. I’m an epidemiologist at Incheon City. I can’t remember everything. Please say what you remember. I’m here to help you go through what you can remember.
[Soundbite]
(Infected person): There were a lot of places I visited...
[Soundbite]
Jang Han-aram (Epidemiologist): You’re sorry? You didn’t have any symptoms. How would you have known? You don’t need to be sorry. We’re grateful that you’ve been diagnosed so that we can prevent further infections.
Seasoned epidemiologists know how to make infected people feel at ease and convince them to cooperate.
[Soundbite]
Jang Han-aram (Epidemiologist): I think it is out of fear. They feel pressure to have their disease confirmed and their itinerary revealed. Many people still view COVID-19 patients in a negative light. They are afraid people will criticize them if their movements are disclosed. They end up hiding the truth because of the criticism.
[Soundbite]
(Worker at logistics center): When I asked what was going on, they told me a person was confirmed. I asked when and where but they said they couldn't say. That person worked at the packaging line on the 12th, I found out through the news that one of my co-workers had tested positive.
This woman contracted the virus even though she followed prevention rules. Her husband also ended up testing positive for COVID-19. If only the truth had been told, if only the critical time had not been lost, this family wouldn’t be in this distress.
[Soundbite]
Honey, wake up. Everyone else is up and all right. You’re the only one lying in bed. Your daughter and I are all here. Honey, can you hear me? Please, wake up.
[Soundbite]
Jang Han-aram (Epidemiologist): When patients are diagnosed with COVID-19, they must feel scared and frustrated. Cooperating with epidemiologists is the only way to protect themselves and people around them. We’re not trying to force information out of you. This is necessary to protect people you care about. Please, understand that.
[Soundbite]
(Epidemiologist at public health center): You cannot go into the hallway or use the elevator. Basically, you won’t be able to leave the room.
The average duration of a phone call with an infected patient is one hour. It’s intensive emotional labor.
[Soundbite]
Jang Han-aram (Epidemiologist): We’re seeing a new spike in COVID-19 cases. A growing number of people are refusing to cooperate with the investigators. In that case, epidemiologists have no choice but to bring up punishment or penalty. Some people even accuse the state of threatening and oppressing them. In extreme cases, they even slander my parents. It’s very discouraging. We conduct these investigations to protect infected patients and their loved ones. But they see me as an oppressor...
It’s been nine months since the COVID-19 pandemic began. Epidemiologists say they have hit a limit, both mentally and physically.
[Soundbite]
Park Eun-jeong (Epidemiologist at public health center): New cases occur randomly, day and night. I have to work until dawn, and I’m sleep-deprived.
The level of stress is hard to express in words.
[Soundbite]
Jang Han-aram (Epidemiologist): I started smoking after I began epidemiological investigations. I also drink a lot of coffee. This is how I relieve stress. Your faith and trust in people gets shattered. You become disappointed and even angry, and that’s how stress keeps building up.
According to a study, epidemiologists experienced the most frustration among jobs related to COVID-19. They were also found to experience above-average levels of mental exhaustion, reaching the state of burnout.
[Soundbite]
Jang Han-aram (Epidemiologist): I want to go camping. I want to set up a tent somewhere quiet and eat alone, enjoying the sound of a stream.
Epidemiologists are still battling COVID-19 on the front line. Even 24 hours a day is not enough to accomplish their task.
■ 제보하기
▷ 카카오톡 : 'KBS제보' 검색, 채널 추가
▷ 전화 : 02-781-1234, 4444
▷ 이메일 : kbs1234@kbs.co.kr
▷ 유튜브, 네이버, 카카오에서도 KBS뉴스를 구독해주세요!
- COVID-19 Trackers
-
- 입력 2020-10-09 14:57:52
- 수정2020-10-09 16:45:41
[Pkg]
Twenty-two COVID-19 cases were confirmed in a building in Seoul on March 8. Epidemiological investigators were the first to be dispatched to the scene.
[Soundbite]
Kim Mi (Epidemiologist): All of a sudden, there were seven to eight media reports daily. I was taken aback. The surveillance camera footage of the freight elevator showed that most people inside it weren’t wearing masks. We concluded it was a critical situation. We ordered the shutdown of the eleventh floor, where the call center is located. We set up a screening station on the first floor and began to test people aggressively.
Some 16-thousand people in the vicinity received an emergency text message. Thanks to a swift investigation that traced the source of infections and close contacts, epidemiologists were able to stop the spread.
We met with the epidemiologist who was at the front line of the COVID-19 response at the time.
[Soundbite]
Jang Han-aram (Epidemiologist): It was the first cluster infection in the Seoul metropolitan area. Obtaining the list of people who were in the building and their contacts, and placing them under self-quarantine quickly made it possible to stop the spread of the virus. I think the epidemiological investigation was deeply meaningful.
A new case was confirmed at dawn. First, the infected persons’ movements are traced through their testimonies.
[Soundbite]
Kim Seong-gon (Epidemiologist): Did you stay home on September 6, 7, and 8?
[Soundbite]
Park Dae-gyu (Epidemiologist): Do any of the employees have a fever or respiratory symptoms? You met with three people?
The whiteboard is filled with information on infections.
[Soundbite]
Jang Han-aram (Epidemiologist): They must have visited a nursing home on August 30 and in early September. I think we’ll have to look into that. Trace their movements before September 3. Get a list of people and start contacting them. Then classify the contacts right away.
While the investigators trace the transmission and identify close contacts, epidemiologists visit the site of the outbreak.
[Soundbite]
Why are you going there?
[Soundbite]
Jang Han-aram (Epidemiologist): There are 2 infected patients at a nursing home. They contracted the virus through different routes. I’m going to find out if those two cases are related. We have to find out the patients’ movements within the hospital, the time of their hospitalization and discharge, and their contacts and transmission routes. We must also assess the risk to decide what measures to take regarding the facility, patients and the staff. That’s why I’m going there.
[Soundbite]
How many epidemiologists are there in your team?
[Soundbite]
Jang Han-aram (Epidemiologist): We had 6 before. But as cases spiked in the capital area, we have 12 now. 4 epidemiologists work every day. We can forecast the number of cases in Incheon. We thought 4 epidemiologists a day could handle that number, so we recruited 6 more people.
This is the nursing home where patients have tested positive for COVID-19. Fast response is critical to mitigating the spread of COVID-19.
[Soundbite]
I should take a picture of this.
[Soundbite]
Kim Seong-gon (Epidemiologist): The nursing home will likely be placed under quarantine. Because it’s a hospital and a high-risk facility, it could be locked down if there are too many infected people and close contacts.
The most critical time is two days before a patient develops first symptoms and right before they are admitted to a hospital. It’s the most infectious period. Prior to an investigation, it’s essential to put on a protective suit, a mask and gloves.
[Soundbite]
Jang Han-aram (Epidemiologist): Check the list of patients, and identify employees who are currently working and patients who were discharged between August 25 and September 9. And the two of you go check surveillance camera footage. Start with the patient who was admitted on August 25.
That day, the epidemiologists managed to prevent additional spread by surveying around 800 people - doctors, patients, vendors and visitors who crossed paths with the infected. We were no longer allowed to continue filming due to transmission concerns.
[Soundbite]
Have you had dinner?
[Soundbite]
Jang Han-aram (Epidemiologist): I grabbed a bite near the hospital after finishing the investigation. I had no time to have lunch. The investigation ended at 5 p.m. Epidemiologists have to work in gowns, face shields, and gloves. Once you’re in, it’s hard to take a break. It’s a hassle to get changed, so once we start, we don’t have meals until we finish.
Epidemiologists of Incheon City work in teams of four, rotating in three shifts around the clock.
[Soundbite]
Jang Han-aram (Epidemiologist): People who visit places where an infected person was at the same time are classified as “contacts.” Classifying and tracing contacts is the purpose of epidemiological studies. We identify contacts, test them and place them under quarantine. Contacts of COVID-19 cases can develop symptoms and become infectious any time. We quarantine them in advance to prevent transmission.
[Soundbite]
In the first stage, we find out when an infected person first developed symptoms. We trace their movements and contacts from two days before that time. Then, we wait for the GPS data. Once we receive it, we check with the patient to reconfirm the route. We do this to identify contacts once again (based on the GPS data).
[Soundbite]
Infected persons do not know who they came across when they visited a public facility. In that case, epidemiologists contact a public health center in the region that the infected person visited, and visit the area to check surveillance camera footage. They ask the health center to identify contacts and conduct tests along with active monitoring.
Back in May, a cluster outbreak occurred at a nightclub in Itaewon. A private academy instructor who was at the club that night lied about his itinerary, but the truth was revealed through an epidemiological study.
[Soundbite]
The GPS data is completely different from the patient’s testimony. He visited the Hongik University area and said he was unemployed, but his friends say he has a job. From the GPS data it’s clear he works near a supermarket.
[Soundbite]
Jang Han-aram (Epidemiologist): It was very frustrating, and dangerous, too. When the academy instructor tested positive, he was highly infectious, but his close contacts slipped through the net. It was a grave situation, so we took immediate action.
[Soundbite]
An Incheon academy instructor who had visited an Itaewon nightclub has caused a septenary infection. The instructor’s student, customers of a singing room, guests at a birthday party, and restaurant customers have contracted the virus. The virus also spread to another restaurant, infecting another customer and family members.
Because of the instructor’s false testimony, his students also became infected.
[Soundbite]
(Patient of secondary transmission): All because of that single lie...I wondered why he had to lie.
One hundred and 25 schools were closed. When infected people lie, the consequences can be quite serious. Encouraging them to tell the truth is critical.
[Soundbite]
Jang Han-aram (Epidemiologist): Hello. I’m an epidemiologist at Incheon City. I can’t remember everything. Please say what you remember. I’m here to help you go through what you can remember.
[Soundbite]
(Infected person): There were a lot of places I visited...
[Soundbite]
Jang Han-aram (Epidemiologist): You’re sorry? You didn’t have any symptoms. How would you have known? You don’t need to be sorry. We’re grateful that you’ve been diagnosed so that we can prevent further infections.
Seasoned epidemiologists know how to make infected people feel at ease and convince them to cooperate.
[Soundbite]
Jang Han-aram (Epidemiologist): I think it is out of fear. They feel pressure to have their disease confirmed and their itinerary revealed. Many people still view COVID-19 patients in a negative light. They are afraid people will criticize them if their movements are disclosed. They end up hiding the truth because of the criticism.
[Soundbite]
(Worker at logistics center): When I asked what was going on, they told me a person was confirmed. I asked when and where but they said they couldn't say. That person worked at the packaging line on the 12th, I found out through the news that one of my co-workers had tested positive.
This woman contracted the virus even though she followed prevention rules. Her husband also ended up testing positive for COVID-19. If only the truth had been told, if only the critical time had not been lost, this family wouldn’t be in this distress.
[Soundbite]
Honey, wake up. Everyone else is up and all right. You’re the only one lying in bed. Your daughter and I are all here. Honey, can you hear me? Please, wake up.
[Soundbite]
Jang Han-aram (Epidemiologist): When patients are diagnosed with COVID-19, they must feel scared and frustrated. Cooperating with epidemiologists is the only way to protect themselves and people around them. We’re not trying to force information out of you. This is necessary to protect people you care about. Please, understand that.
[Soundbite]
(Epidemiologist at public health center): You cannot go into the hallway or use the elevator. Basically, you won’t be able to leave the room.
The average duration of a phone call with an infected patient is one hour. It’s intensive emotional labor.
[Soundbite]
Jang Han-aram (Epidemiologist): We’re seeing a new spike in COVID-19 cases. A growing number of people are refusing to cooperate with the investigators. In that case, epidemiologists have no choice but to bring up punishment or penalty. Some people even accuse the state of threatening and oppressing them. In extreme cases, they even slander my parents. It’s very discouraging. We conduct these investigations to protect infected patients and their loved ones. But they see me as an oppressor...
It’s been nine months since the COVID-19 pandemic began. Epidemiologists say they have hit a limit, both mentally and physically.
[Soundbite]
Park Eun-jeong (Epidemiologist at public health center): New cases occur randomly, day and night. I have to work until dawn, and I’m sleep-deprived.
The level of stress is hard to express in words.
[Soundbite]
Jang Han-aram (Epidemiologist): I started smoking after I began epidemiological investigations. I also drink a lot of coffee. This is how I relieve stress. Your faith and trust in people gets shattered. You become disappointed and even angry, and that’s how stress keeps building up.
According to a study, epidemiologists experienced the most frustration among jobs related to COVID-19. They were also found to experience above-average levels of mental exhaustion, reaching the state of burnout.
[Soundbite]
Jang Han-aram (Epidemiologist): I want to go camping. I want to set up a tent somewhere quiet and eat alone, enjoying the sound of a stream.
Epidemiologists are still battling COVID-19 on the front line. Even 24 hours a day is not enough to accomplish their task.
Twenty-two COVID-19 cases were confirmed in a building in Seoul on March 8. Epidemiological investigators were the first to be dispatched to the scene.
[Soundbite]
Kim Mi (Epidemiologist): All of a sudden, there were seven to eight media reports daily. I was taken aback. The surveillance camera footage of the freight elevator showed that most people inside it weren’t wearing masks. We concluded it was a critical situation. We ordered the shutdown of the eleventh floor, where the call center is located. We set up a screening station on the first floor and began to test people aggressively.
Some 16-thousand people in the vicinity received an emergency text message. Thanks to a swift investigation that traced the source of infections and close contacts, epidemiologists were able to stop the spread.
We met with the epidemiologist who was at the front line of the COVID-19 response at the time.
[Soundbite]
Jang Han-aram (Epidemiologist): It was the first cluster infection in the Seoul metropolitan area. Obtaining the list of people who were in the building and their contacts, and placing them under self-quarantine quickly made it possible to stop the spread of the virus. I think the epidemiological investigation was deeply meaningful.
A new case was confirmed at dawn. First, the infected persons’ movements are traced through their testimonies.
[Soundbite]
Kim Seong-gon (Epidemiologist): Did you stay home on September 6, 7, and 8?
[Soundbite]
Park Dae-gyu (Epidemiologist): Do any of the employees have a fever or respiratory symptoms? You met with three people?
The whiteboard is filled with information on infections.
[Soundbite]
Jang Han-aram (Epidemiologist): They must have visited a nursing home on August 30 and in early September. I think we’ll have to look into that. Trace their movements before September 3. Get a list of people and start contacting them. Then classify the contacts right away.
While the investigators trace the transmission and identify close contacts, epidemiologists visit the site of the outbreak.
[Soundbite]
Why are you going there?
[Soundbite]
Jang Han-aram (Epidemiologist): There are 2 infected patients at a nursing home. They contracted the virus through different routes. I’m going to find out if those two cases are related. We have to find out the patients’ movements within the hospital, the time of their hospitalization and discharge, and their contacts and transmission routes. We must also assess the risk to decide what measures to take regarding the facility, patients and the staff. That’s why I’m going there.
[Soundbite]
How many epidemiologists are there in your team?
[Soundbite]
Jang Han-aram (Epidemiologist): We had 6 before. But as cases spiked in the capital area, we have 12 now. 4 epidemiologists work every day. We can forecast the number of cases in Incheon. We thought 4 epidemiologists a day could handle that number, so we recruited 6 more people.
This is the nursing home where patients have tested positive for COVID-19. Fast response is critical to mitigating the spread of COVID-19.
[Soundbite]
I should take a picture of this.
[Soundbite]
Kim Seong-gon (Epidemiologist): The nursing home will likely be placed under quarantine. Because it’s a hospital and a high-risk facility, it could be locked down if there are too many infected people and close contacts.
The most critical time is two days before a patient develops first symptoms and right before they are admitted to a hospital. It’s the most infectious period. Prior to an investigation, it’s essential to put on a protective suit, a mask and gloves.
[Soundbite]
Jang Han-aram (Epidemiologist): Check the list of patients, and identify employees who are currently working and patients who were discharged between August 25 and September 9. And the two of you go check surveillance camera footage. Start with the patient who was admitted on August 25.
That day, the epidemiologists managed to prevent additional spread by surveying around 800 people - doctors, patients, vendors and visitors who crossed paths with the infected. We were no longer allowed to continue filming due to transmission concerns.
[Soundbite]
Have you had dinner?
[Soundbite]
Jang Han-aram (Epidemiologist): I grabbed a bite near the hospital after finishing the investigation. I had no time to have lunch. The investigation ended at 5 p.m. Epidemiologists have to work in gowns, face shields, and gloves. Once you’re in, it’s hard to take a break. It’s a hassle to get changed, so once we start, we don’t have meals until we finish.
Epidemiologists of Incheon City work in teams of four, rotating in three shifts around the clock.
[Soundbite]
Jang Han-aram (Epidemiologist): People who visit places where an infected person was at the same time are classified as “contacts.” Classifying and tracing contacts is the purpose of epidemiological studies. We identify contacts, test them and place them under quarantine. Contacts of COVID-19 cases can develop symptoms and become infectious any time. We quarantine them in advance to prevent transmission.
[Soundbite]
In the first stage, we find out when an infected person first developed symptoms. We trace their movements and contacts from two days before that time. Then, we wait for the GPS data. Once we receive it, we check with the patient to reconfirm the route. We do this to identify contacts once again (based on the GPS data).
[Soundbite]
Infected persons do not know who they came across when they visited a public facility. In that case, epidemiologists contact a public health center in the region that the infected person visited, and visit the area to check surveillance camera footage. They ask the health center to identify contacts and conduct tests along with active monitoring.
Back in May, a cluster outbreak occurred at a nightclub in Itaewon. A private academy instructor who was at the club that night lied about his itinerary, but the truth was revealed through an epidemiological study.
[Soundbite]
The GPS data is completely different from the patient’s testimony. He visited the Hongik University area and said he was unemployed, but his friends say he has a job. From the GPS data it’s clear he works near a supermarket.
[Soundbite]
Jang Han-aram (Epidemiologist): It was very frustrating, and dangerous, too. When the academy instructor tested positive, he was highly infectious, but his close contacts slipped through the net. It was a grave situation, so we took immediate action.
[Soundbite]
An Incheon academy instructor who had visited an Itaewon nightclub has caused a septenary infection. The instructor’s student, customers of a singing room, guests at a birthday party, and restaurant customers have contracted the virus. The virus also spread to another restaurant, infecting another customer and family members.
Because of the instructor’s false testimony, his students also became infected.
[Soundbite]
(Patient of secondary transmission): All because of that single lie...I wondered why he had to lie.
One hundred and 25 schools were closed. When infected people lie, the consequences can be quite serious. Encouraging them to tell the truth is critical.
[Soundbite]
Jang Han-aram (Epidemiologist): Hello. I’m an epidemiologist at Incheon City. I can’t remember everything. Please say what you remember. I’m here to help you go through what you can remember.
[Soundbite]
(Infected person): There were a lot of places I visited...
[Soundbite]
Jang Han-aram (Epidemiologist): You’re sorry? You didn’t have any symptoms. How would you have known? You don’t need to be sorry. We’re grateful that you’ve been diagnosed so that we can prevent further infections.
Seasoned epidemiologists know how to make infected people feel at ease and convince them to cooperate.
[Soundbite]
Jang Han-aram (Epidemiologist): I think it is out of fear. They feel pressure to have their disease confirmed and their itinerary revealed. Many people still view COVID-19 patients in a negative light. They are afraid people will criticize them if their movements are disclosed. They end up hiding the truth because of the criticism.
[Soundbite]
(Worker at logistics center): When I asked what was going on, they told me a person was confirmed. I asked when and where but they said they couldn't say. That person worked at the packaging line on the 12th, I found out through the news that one of my co-workers had tested positive.
This woman contracted the virus even though she followed prevention rules. Her husband also ended up testing positive for COVID-19. If only the truth had been told, if only the critical time had not been lost, this family wouldn’t be in this distress.
[Soundbite]
Honey, wake up. Everyone else is up and all right. You’re the only one lying in bed. Your daughter and I are all here. Honey, can you hear me? Please, wake up.
[Soundbite]
Jang Han-aram (Epidemiologist): When patients are diagnosed with COVID-19, they must feel scared and frustrated. Cooperating with epidemiologists is the only way to protect themselves and people around them. We’re not trying to force information out of you. This is necessary to protect people you care about. Please, understand that.
[Soundbite]
(Epidemiologist at public health center): You cannot go into the hallway or use the elevator. Basically, you won’t be able to leave the room.
The average duration of a phone call with an infected patient is one hour. It’s intensive emotional labor.
[Soundbite]
Jang Han-aram (Epidemiologist): We’re seeing a new spike in COVID-19 cases. A growing number of people are refusing to cooperate with the investigators. In that case, epidemiologists have no choice but to bring up punishment or penalty. Some people even accuse the state of threatening and oppressing them. In extreme cases, they even slander my parents. It’s very discouraging. We conduct these investigations to protect infected patients and their loved ones. But they see me as an oppressor...
It’s been nine months since the COVID-19 pandemic began. Epidemiologists say they have hit a limit, both mentally and physically.
[Soundbite]
Park Eun-jeong (Epidemiologist at public health center): New cases occur randomly, day and night. I have to work until dawn, and I’m sleep-deprived.
The level of stress is hard to express in words.
[Soundbite]
Jang Han-aram (Epidemiologist): I started smoking after I began epidemiological investigations. I also drink a lot of coffee. This is how I relieve stress. Your faith and trust in people gets shattered. You become disappointed and even angry, and that’s how stress keeps building up.
According to a study, epidemiologists experienced the most frustration among jobs related to COVID-19. They were also found to experience above-average levels of mental exhaustion, reaching the state of burnout.
[Soundbite]
Jang Han-aram (Epidemiologist): I want to go camping. I want to set up a tent somewhere quiet and eat alone, enjoying the sound of a stream.
Epidemiologists are still battling COVID-19 on the front line. Even 24 hours a day is not enough to accomplish their task.
이 기사가 좋으셨다면
-
좋아요
0
-
응원해요
0
-
후속 원해요
0














이 기사에 대한 의견을 남겨주세요.