Endless Battle against COVID-19
입력 2020.12.25 (16:47)
수정 2020.12.25 (17:20)
읽어주기 기능은 크롬기반의
브라우저에서만 사용하실 수 있습니다.
[Pkg]
[Soundbite]
The nation has added 1,062 more COVID-19 cases. The daily tally has been at over one thousand for three days in a row.
It’s been 340 days since the first COVID-19 case in South Korea. The war against the virus is still on. Soaring cases, shortage of hospital beds, exhausted medical workers. The world is fighting the third wave of the novel coronavirus, and the outcome is unpredictable. How is Korea dealing with the third wave of infections, and what can be done to adapt to the new normal era of living with the coronavirus?
[Soundbite]
Choi Young-il (Social critic): Let's talk about Korea’s quarantine crisis. K-quarantine. The nation earned global acclaim through public participation and set an example for the world. The third wave began in November. Unlike the previous two waves, it presented a tremendous challenge to K-quarantine. Joining us today are Professor Ki Mo-ran from the Korean Society for Preventive Medicine and Professor Lee Jae-gap from Hallym University Infectious Disease Department.
A long line of people waiting to get tested for COVID-19. The number of coronavirus cases in Korea has soared lately. What’s most concerning is that the third wave of infections is different from the previous two.
[Soundbite]
Jung Eun-kyeong (Director of KDCA): In the past, coronavirus cases mostly occurred in the capital area, in select groups. But nowadays they are spreading in other regions as well through daily activities in various groups.
The first wave of COVID-19 in Korea began at Sincheonji Church and occurred mostly in Daegu and Gyeongsangbuk-do Province. The second wave spread at rallies and religious facilities in the Seoul metropolitan area. The third wave, however, does not involve massive outbreaks in certain areas or groups, and has spread evenly to every corner of the nation. The silent spread of COVID-19 has permeated daily life in every corner of the country. What can be done to stop it?
[Soundbite]
Choi Young-il (Social critic): Let’s discuss this further with Professor Lee Jae-gap.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Hello.
[Soundbite]
Choi Young-il (Social critic): In your opinion, what is the leading cause of the third wave of COVID-19?
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): COVID-19 is relentlessly spreading through local communities. The biggest factor is the season. As the weather gets cold, people spend more time indoors. This will likely contribute to continued large-scale spread.
[Soundbite]
Choi Young-il (Social critic): We’re standing at a critical juncture. There's been many days with over 1,000 new cases. We’re seeing hundreds of cases daily, and they need to be hospitalized. Some of them have serious symptoms and the death toll has been rising recently. Shortage of hospital beds is one of the most concerning issue these days.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): As of December 17, about 40 ICU beds were available nationwide. Quarantine centers and infectious disease hospitals are around 70 percent full. The government is trying to secure 300 ICUs by early 2021 and provide 7,000-10,000 more hospital beds. ICU patients are the greatest concern. Hospitals could run out of ICU beds within a couple of weeks. We must secure more ICU beds at general hospitals, university medical centers or private hospitals as soon as possible.
[Soundbite]
Choi Young-il (Social critic): Let’s hear from Professor Ki Mo-ran. Hello, Professor. Concerns grow over the shortage of hospital beds in the capital area. What measures has the government devised to address the situation?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): So far, COVID-19 patients have been treated at public hospitals. But it’s not enough. We are asking private hospitals to help. Some hospitals have agreed to treat COVID-19 patients. But we need more such cooperation to solve bed shortages.
[Soundbite]
Choi Young-il (Social critic): The outbreak is becoming very protracted. It’s been almost a year now. The primary concern is health workers’ burnout and the shortage of nurses. Professor Lee, you probably know better than anyone what the health workers are going through.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): It’s a tough time for medical workers. But they continue doing their job because patients need them. I am worried they will be pushed to their limits if there are too many patients. All medical workers are urging the public to follow social distancing rules to reduce the number of patients so that nobody is rejected hospital treatment and all ICU patients can receive help.
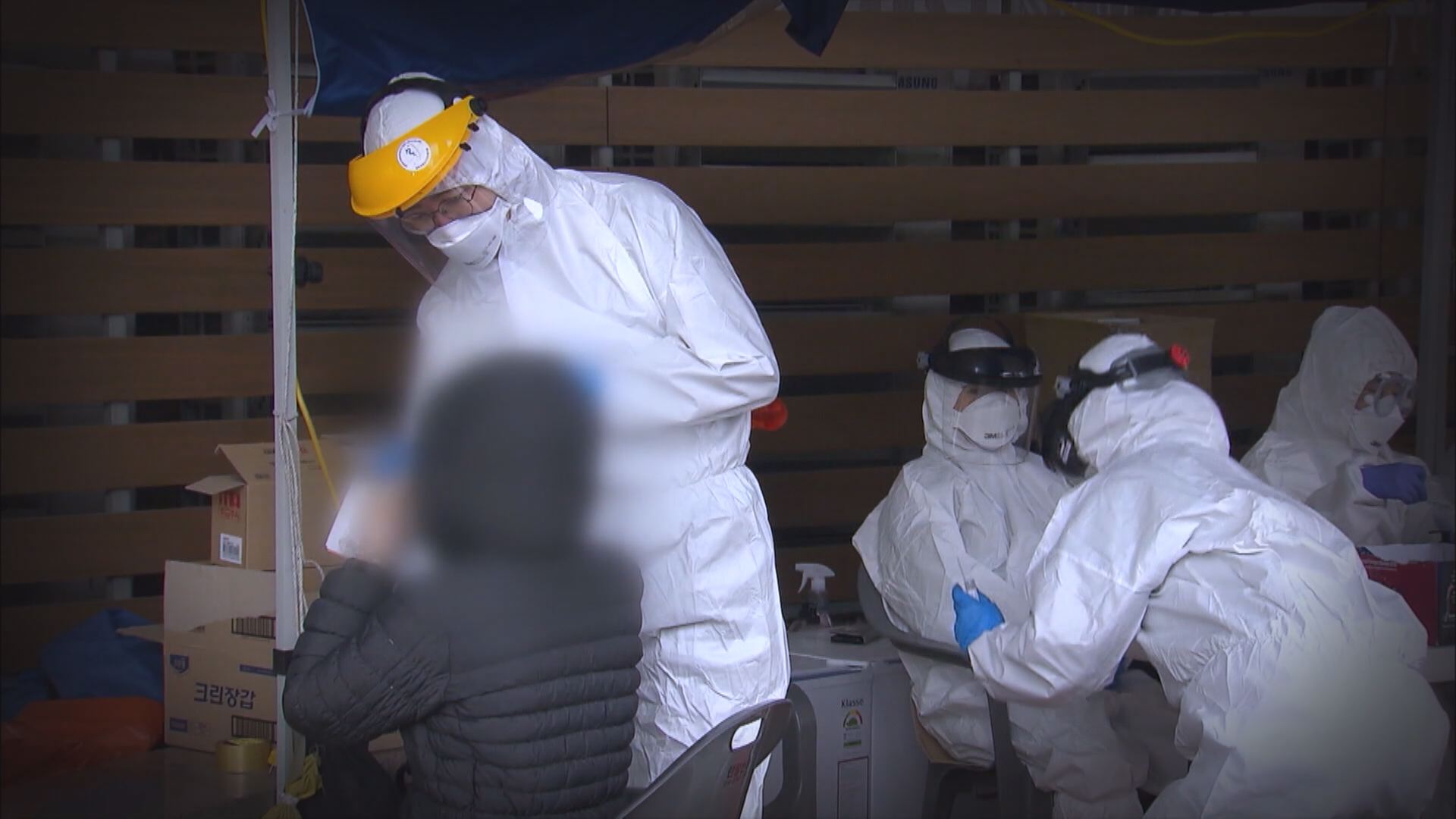
This public hospital in Incheon has eleven ICU beds, but only four of them can be operated.
[Soundbite]
Cho Seung-yeon (Director of Incheon Medical Center): To treat seven more ICU patients, we need five doctors and 15-20 nurses.
Medical workers taking care of critically ill COVID-19 patients must wear Level D hazmat suits and work around the clock in shifts. This means more nurses are required than for other ICU patients.
[Soundbite]
Choi Young-il (Social critic): The question is how medical workers can be rewarded and encouraged to do their job. Of course, financial reward is an option. But the most fundamental solution is expanding the number of health workers. What do you think, Professor?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): Financial reward is one of the ways to do it. What needs to be done eventually is reducing workload. Nurses and medical technologists should be allowed to perform doctors’ duties. The number of medical personnel should be increased. If social distancing measures are raised and many facilities close down, the social cost will be enormous. It’d be more efficient to hire and train more health workers so that more patients can receive treatment.
[Soundbite]
Choi Young-il (Social critic): The protracted pandemic has resulted in shortage of beds
and health workers’ burnout. Many experts say the ultimate game changer will be a vaccine. U.S. President Donald Trump recently issued an executive order to administer vaccines to the American public first. Many in Korea worry that the country’s efforts to buy and provide vaccines could be stymied. What’s your take on this?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It’s been almost a year since the COVID-19 pandemic began. Instead of cooperating, each country only cares about its people. The pandemic will not be over if only one country is vaccinated. I hope the U.S. will understand this soon. I don’t think we need to worry about securing vaccines in Korea. First of all, the infection rate in Korea is quite stable compared to the U.S. or the U.K. Some say we must follow Germany and implement a lockdown. Germany has 20 times more cases than Korea. It's a different situation. Once a vaccine is brought to the country, it will be first administered to the residents and workers of high-risk, long-term care facilities. After inoculating about 10 million people, medical workers will be able to treat coronavirus patients with less worry.
[Soundbite]
Choi Young-il (Social critic): Many people in Korea want to know when they will be inoculated. The government at first said vaccination would start in the second quarter or second half of 2021. But lately it moved it up to February-March. Can vaccination begin even earlier than that?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It would be difficult. There must be companies that have already applied or emergency use authorization. t takes more than a month to deliberate vaccine safety.
[Soundbite]
Choi Young-il (Social critic): The development of COVID-19 treatments is also a major concern, because infected patients need to be treated as soon as possible. Korean companies such as Celltrion and Green Cross are also developing coronavirus treatments. When can they be utilized to treat patients?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The antibody treatment developed by Celltrion can be utilized soon. The results of Phase 2 clinical trials are to be released soon. Then the company can apply for emergency use authorization. If the treatment is approved before Phase 3 trials, it will be utilized within this year. Clinical trials are conducted on patients to prevent further aggravation of symptoms. Once safety is verified, treatments can be approved for immediate use even if their efficacy is somewhat low.
[Soundbite]
Choi Young-il (Social critic): COVID-19 is a new virus different from anything we've experienced before. Nobody knows if it can be eradicated. Then how should we change our lives to live with this virus?
[Soundbite]
Jung Eun-kyeong (Director of KDCA): Ironically, the only way to join hands in the era of COVID-19 is to stay apart and maintain a safe distance. Coronavirus is invisible, but it is spread continuously and survives when people meet. We can stop the spread if we avoid contact with others.
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The COVID-19 pandemic has changed the world as we know it. It is a crisis. But to some, it’s an opportunity. In times like these, we must lend a helping hand to those in need so that we can beat the virus together.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Viruses, bacteria and microorganisms will continue to threaten humans in the future. During outbreaks of infectious diseases, the most vulnerable groups in our society are most adversely affected by it. We need to find ways to better protect them. COVID-19 has profoundly changed our society. We can make our country safe and become the most successful nation in fighting COVID-19 five to ten years from now if we adapt to these changes and work together.
[Soundbite]
Choi Young-il (Social critic): We can beat COVID-19 only through social distancing, wearing masks and following precautions thoroughly. There are no shortcuts. It’s important to keep in mind that each individual’s ill-advised actions can put an entire community at risk.
After a long fight against COVID-19, Korea’s quarantine efforts seem to be losing ground. However this pandemic has taught us that we can beat this virus only if the public, medical workers and the government join hands under the common goal.
[Soundbite]
The nation has added 1,062 more COVID-19 cases. The daily tally has been at over one thousand for three days in a row.
It’s been 340 days since the first COVID-19 case in South Korea. The war against the virus is still on. Soaring cases, shortage of hospital beds, exhausted medical workers. The world is fighting the third wave of the novel coronavirus, and the outcome is unpredictable. How is Korea dealing with the third wave of infections, and what can be done to adapt to the new normal era of living with the coronavirus?
[Soundbite]
Choi Young-il (Social critic): Let's talk about Korea’s quarantine crisis. K-quarantine. The nation earned global acclaim through public participation and set an example for the world. The third wave began in November. Unlike the previous two waves, it presented a tremendous challenge to K-quarantine. Joining us today are Professor Ki Mo-ran from the Korean Society for Preventive Medicine and Professor Lee Jae-gap from Hallym University Infectious Disease Department.
A long line of people waiting to get tested for COVID-19. The number of coronavirus cases in Korea has soared lately. What’s most concerning is that the third wave of infections is different from the previous two.
[Soundbite]
Jung Eun-kyeong (Director of KDCA): In the past, coronavirus cases mostly occurred in the capital area, in select groups. But nowadays they are spreading in other regions as well through daily activities in various groups.
The first wave of COVID-19 in Korea began at Sincheonji Church and occurred mostly in Daegu and Gyeongsangbuk-do Province. The second wave spread at rallies and religious facilities in the Seoul metropolitan area. The third wave, however, does not involve massive outbreaks in certain areas or groups, and has spread evenly to every corner of the nation. The silent spread of COVID-19 has permeated daily life in every corner of the country. What can be done to stop it?
[Soundbite]
Choi Young-il (Social critic): Let’s discuss this further with Professor Lee Jae-gap.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Hello.
[Soundbite]
Choi Young-il (Social critic): In your opinion, what is the leading cause of the third wave of COVID-19?
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): COVID-19 is relentlessly spreading through local communities. The biggest factor is the season. As the weather gets cold, people spend more time indoors. This will likely contribute to continued large-scale spread.
[Soundbite]
Choi Young-il (Social critic): We’re standing at a critical juncture. There's been many days with over 1,000 new cases. We’re seeing hundreds of cases daily, and they need to be hospitalized. Some of them have serious symptoms and the death toll has been rising recently. Shortage of hospital beds is one of the most concerning issue these days.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): As of December 17, about 40 ICU beds were available nationwide. Quarantine centers and infectious disease hospitals are around 70 percent full. The government is trying to secure 300 ICUs by early 2021 and provide 7,000-10,000 more hospital beds. ICU patients are the greatest concern. Hospitals could run out of ICU beds within a couple of weeks. We must secure more ICU beds at general hospitals, university medical centers or private hospitals as soon as possible.
[Soundbite]
Choi Young-il (Social critic): Let’s hear from Professor Ki Mo-ran. Hello, Professor. Concerns grow over the shortage of hospital beds in the capital area. What measures has the government devised to address the situation?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): So far, COVID-19 patients have been treated at public hospitals. But it’s not enough. We are asking private hospitals to help. Some hospitals have agreed to treat COVID-19 patients. But we need more such cooperation to solve bed shortages.
[Soundbite]
Choi Young-il (Social critic): The outbreak is becoming very protracted. It’s been almost a year now. The primary concern is health workers’ burnout and the shortage of nurses. Professor Lee, you probably know better than anyone what the health workers are going through.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): It’s a tough time for medical workers. But they continue doing their job because patients need them. I am worried they will be pushed to their limits if there are too many patients. All medical workers are urging the public to follow social distancing rules to reduce the number of patients so that nobody is rejected hospital treatment and all ICU patients can receive help.
This public hospital in Incheon has eleven ICU beds, but only four of them can be operated.
[Soundbite]
Cho Seung-yeon (Director of Incheon Medical Center): To treat seven more ICU patients, we need five doctors and 15-20 nurses.
Medical workers taking care of critically ill COVID-19 patients must wear Level D hazmat suits and work around the clock in shifts. This means more nurses are required than for other ICU patients.
[Soundbite]
Choi Young-il (Social critic): The question is how medical workers can be rewarded and encouraged to do their job. Of course, financial reward is an option. But the most fundamental solution is expanding the number of health workers. What do you think, Professor?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): Financial reward is one of the ways to do it. What needs to be done eventually is reducing workload. Nurses and medical technologists should be allowed to perform doctors’ duties. The number of medical personnel should be increased. If social distancing measures are raised and many facilities close down, the social cost will be enormous. It’d be more efficient to hire and train more health workers so that more patients can receive treatment.
[Soundbite]
Choi Young-il (Social critic): The protracted pandemic has resulted in shortage of beds
and health workers’ burnout. Many experts say the ultimate game changer will be a vaccine. U.S. President Donald Trump recently issued an executive order to administer vaccines to the American public first. Many in Korea worry that the country’s efforts to buy and provide vaccines could be stymied. What’s your take on this?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It’s been almost a year since the COVID-19 pandemic began. Instead of cooperating, each country only cares about its people. The pandemic will not be over if only one country is vaccinated. I hope the U.S. will understand this soon. I don’t think we need to worry about securing vaccines in Korea. First of all, the infection rate in Korea is quite stable compared to the U.S. or the U.K. Some say we must follow Germany and implement a lockdown. Germany has 20 times more cases than Korea. It's a different situation. Once a vaccine is brought to the country, it will be first administered to the residents and workers of high-risk, long-term care facilities. After inoculating about 10 million people, medical workers will be able to treat coronavirus patients with less worry.
[Soundbite]
Choi Young-il (Social critic): Many people in Korea want to know when they will be inoculated. The government at first said vaccination would start in the second quarter or second half of 2021. But lately it moved it up to February-March. Can vaccination begin even earlier than that?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It would be difficult. There must be companies that have already applied or emergency use authorization. t takes more than a month to deliberate vaccine safety.
[Soundbite]
Choi Young-il (Social critic): The development of COVID-19 treatments is also a major concern, because infected patients need to be treated as soon as possible. Korean companies such as Celltrion and Green Cross are also developing coronavirus treatments. When can they be utilized to treat patients?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The antibody treatment developed by Celltrion can be utilized soon. The results of Phase 2 clinical trials are to be released soon. Then the company can apply for emergency use authorization. If the treatment is approved before Phase 3 trials, it will be utilized within this year. Clinical trials are conducted on patients to prevent further aggravation of symptoms. Once safety is verified, treatments can be approved for immediate use even if their efficacy is somewhat low.
[Soundbite]
Choi Young-il (Social critic): COVID-19 is a new virus different from anything we've experienced before. Nobody knows if it can be eradicated. Then how should we change our lives to live with this virus?
[Soundbite]
Jung Eun-kyeong (Director of KDCA): Ironically, the only way to join hands in the era of COVID-19 is to stay apart and maintain a safe distance. Coronavirus is invisible, but it is spread continuously and survives when people meet. We can stop the spread if we avoid contact with others.
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The COVID-19 pandemic has changed the world as we know it. It is a crisis. But to some, it’s an opportunity. In times like these, we must lend a helping hand to those in need so that we can beat the virus together.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Viruses, bacteria and microorganisms will continue to threaten humans in the future. During outbreaks of infectious diseases, the most vulnerable groups in our society are most adversely affected by it. We need to find ways to better protect them. COVID-19 has profoundly changed our society. We can make our country safe and become the most successful nation in fighting COVID-19 five to ten years from now if we adapt to these changes and work together.
[Soundbite]
Choi Young-il (Social critic): We can beat COVID-19 only through social distancing, wearing masks and following precautions thoroughly. There are no shortcuts. It’s important to keep in mind that each individual’s ill-advised actions can put an entire community at risk.
After a long fight against COVID-19, Korea’s quarantine efforts seem to be losing ground. However this pandemic has taught us that we can beat this virus only if the public, medical workers and the government join hands under the common goal.
■ 제보하기
▷ 카카오톡 : 'KBS제보' 검색, 채널 추가
▷ 전화 : 02-781-1234, 4444
▷ 이메일 : kbs1234@kbs.co.kr
▷ 유튜브, 네이버, 카카오에서도 KBS뉴스를 구독해주세요!
- Endless Battle against COVID-19
-
- 입력 2020-12-25 16:47:35
- 수정2020-12-25 17:20:06
[Pkg]
[Soundbite]
The nation has added 1,062 more COVID-19 cases. The daily tally has been at over one thousand for three days in a row.
It’s been 340 days since the first COVID-19 case in South Korea. The war against the virus is still on. Soaring cases, shortage of hospital beds, exhausted medical workers. The world is fighting the third wave of the novel coronavirus, and the outcome is unpredictable. How is Korea dealing with the third wave of infections, and what can be done to adapt to the new normal era of living with the coronavirus?
[Soundbite]
Choi Young-il (Social critic): Let's talk about Korea’s quarantine crisis. K-quarantine. The nation earned global acclaim through public participation and set an example for the world. The third wave began in November. Unlike the previous two waves, it presented a tremendous challenge to K-quarantine. Joining us today are Professor Ki Mo-ran from the Korean Society for Preventive Medicine and Professor Lee Jae-gap from Hallym University Infectious Disease Department.
A long line of people waiting to get tested for COVID-19. The number of coronavirus cases in Korea has soared lately. What’s most concerning is that the third wave of infections is different from the previous two.
[Soundbite]
Jung Eun-kyeong (Director of KDCA): In the past, coronavirus cases mostly occurred in the capital area, in select groups. But nowadays they are spreading in other regions as well through daily activities in various groups.
The first wave of COVID-19 in Korea began at Sincheonji Church and occurred mostly in Daegu and Gyeongsangbuk-do Province. The second wave spread at rallies and religious facilities in the Seoul metropolitan area. The third wave, however, does not involve massive outbreaks in certain areas or groups, and has spread evenly to every corner of the nation. The silent spread of COVID-19 has permeated daily life in every corner of the country. What can be done to stop it?
[Soundbite]
Choi Young-il (Social critic): Let’s discuss this further with Professor Lee Jae-gap.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Hello.
[Soundbite]
Choi Young-il (Social critic): In your opinion, what is the leading cause of the third wave of COVID-19?
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): COVID-19 is relentlessly spreading through local communities. The biggest factor is the season. As the weather gets cold, people spend more time indoors. This will likely contribute to continued large-scale spread.
[Soundbite]
Choi Young-il (Social critic): We’re standing at a critical juncture. There's been many days with over 1,000 new cases. We’re seeing hundreds of cases daily, and they need to be hospitalized. Some of them have serious symptoms and the death toll has been rising recently. Shortage of hospital beds is one of the most concerning issue these days.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): As of December 17, about 40 ICU beds were available nationwide. Quarantine centers and infectious disease hospitals are around 70 percent full. The government is trying to secure 300 ICUs by early 2021 and provide 7,000-10,000 more hospital beds. ICU patients are the greatest concern. Hospitals could run out of ICU beds within a couple of weeks. We must secure more ICU beds at general hospitals, university medical centers or private hospitals as soon as possible.
[Soundbite]
Choi Young-il (Social critic): Let’s hear from Professor Ki Mo-ran. Hello, Professor. Concerns grow over the shortage of hospital beds in the capital area. What measures has the government devised to address the situation?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): So far, COVID-19 patients have been treated at public hospitals. But it’s not enough. We are asking private hospitals to help. Some hospitals have agreed to treat COVID-19 patients. But we need more such cooperation to solve bed shortages.
[Soundbite]
Choi Young-il (Social critic): The outbreak is becoming very protracted. It’s been almost a year now. The primary concern is health workers’ burnout and the shortage of nurses. Professor Lee, you probably know better than anyone what the health workers are going through.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): It’s a tough time for medical workers. But they continue doing their job because patients need them. I am worried they will be pushed to their limits if there are too many patients. All medical workers are urging the public to follow social distancing rules to reduce the number of patients so that nobody is rejected hospital treatment and all ICU patients can receive help.
This public hospital in Incheon has eleven ICU beds, but only four of them can be operated.
[Soundbite]
Cho Seung-yeon (Director of Incheon Medical Center): To treat seven more ICU patients, we need five doctors and 15-20 nurses.
Medical workers taking care of critically ill COVID-19 patients must wear Level D hazmat suits and work around the clock in shifts. This means more nurses are required than for other ICU patients.
[Soundbite]
Choi Young-il (Social critic): The question is how medical workers can be rewarded and encouraged to do their job. Of course, financial reward is an option. But the most fundamental solution is expanding the number of health workers. What do you think, Professor?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): Financial reward is one of the ways to do it. What needs to be done eventually is reducing workload. Nurses and medical technologists should be allowed to perform doctors’ duties. The number of medical personnel should be increased. If social distancing measures are raised and many facilities close down, the social cost will be enormous. It’d be more efficient to hire and train more health workers so that more patients can receive treatment.
[Soundbite]
Choi Young-il (Social critic): The protracted pandemic has resulted in shortage of beds
and health workers’ burnout. Many experts say the ultimate game changer will be a vaccine. U.S. President Donald Trump recently issued an executive order to administer vaccines to the American public first. Many in Korea worry that the country’s efforts to buy and provide vaccines could be stymied. What’s your take on this?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It’s been almost a year since the COVID-19 pandemic began. Instead of cooperating, each country only cares about its people. The pandemic will not be over if only one country is vaccinated. I hope the U.S. will understand this soon. I don’t think we need to worry about securing vaccines in Korea. First of all, the infection rate in Korea is quite stable compared to the U.S. or the U.K. Some say we must follow Germany and implement a lockdown. Germany has 20 times more cases than Korea. It's a different situation. Once a vaccine is brought to the country, it will be first administered to the residents and workers of high-risk, long-term care facilities. After inoculating about 10 million people, medical workers will be able to treat coronavirus patients with less worry.
[Soundbite]
Choi Young-il (Social critic): Many people in Korea want to know when they will be inoculated. The government at first said vaccination would start in the second quarter or second half of 2021. But lately it moved it up to February-March. Can vaccination begin even earlier than that?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It would be difficult. There must be companies that have already applied or emergency use authorization. t takes more than a month to deliberate vaccine safety.
[Soundbite]
Choi Young-il (Social critic): The development of COVID-19 treatments is also a major concern, because infected patients need to be treated as soon as possible. Korean companies such as Celltrion and Green Cross are also developing coronavirus treatments. When can they be utilized to treat patients?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The antibody treatment developed by Celltrion can be utilized soon. The results of Phase 2 clinical trials are to be released soon. Then the company can apply for emergency use authorization. If the treatment is approved before Phase 3 trials, it will be utilized within this year. Clinical trials are conducted on patients to prevent further aggravation of symptoms. Once safety is verified, treatments can be approved for immediate use even if their efficacy is somewhat low.
[Soundbite]
Choi Young-il (Social critic): COVID-19 is a new virus different from anything we've experienced before. Nobody knows if it can be eradicated. Then how should we change our lives to live with this virus?
[Soundbite]
Jung Eun-kyeong (Director of KDCA): Ironically, the only way to join hands in the era of COVID-19 is to stay apart and maintain a safe distance. Coronavirus is invisible, but it is spread continuously and survives when people meet. We can stop the spread if we avoid contact with others.
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The COVID-19 pandemic has changed the world as we know it. It is a crisis. But to some, it’s an opportunity. In times like these, we must lend a helping hand to those in need so that we can beat the virus together.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Viruses, bacteria and microorganisms will continue to threaten humans in the future. During outbreaks of infectious diseases, the most vulnerable groups in our society are most adversely affected by it. We need to find ways to better protect them. COVID-19 has profoundly changed our society. We can make our country safe and become the most successful nation in fighting COVID-19 five to ten years from now if we adapt to these changes and work together.
[Soundbite]
Choi Young-il (Social critic): We can beat COVID-19 only through social distancing, wearing masks and following precautions thoroughly. There are no shortcuts. It’s important to keep in mind that each individual’s ill-advised actions can put an entire community at risk.
After a long fight against COVID-19, Korea’s quarantine efforts seem to be losing ground. However this pandemic has taught us that we can beat this virus only if the public, medical workers and the government join hands under the common goal.
[Soundbite]
The nation has added 1,062 more COVID-19 cases. The daily tally has been at over one thousand for three days in a row.
It’s been 340 days since the first COVID-19 case in South Korea. The war against the virus is still on. Soaring cases, shortage of hospital beds, exhausted medical workers. The world is fighting the third wave of the novel coronavirus, and the outcome is unpredictable. How is Korea dealing with the third wave of infections, and what can be done to adapt to the new normal era of living with the coronavirus?
[Soundbite]
Choi Young-il (Social critic): Let's talk about Korea’s quarantine crisis. K-quarantine. The nation earned global acclaim through public participation and set an example for the world. The third wave began in November. Unlike the previous two waves, it presented a tremendous challenge to K-quarantine. Joining us today are Professor Ki Mo-ran from the Korean Society for Preventive Medicine and Professor Lee Jae-gap from Hallym University Infectious Disease Department.
A long line of people waiting to get tested for COVID-19. The number of coronavirus cases in Korea has soared lately. What’s most concerning is that the third wave of infections is different from the previous two.
[Soundbite]
Jung Eun-kyeong (Director of KDCA): In the past, coronavirus cases mostly occurred in the capital area, in select groups. But nowadays they are spreading in other regions as well through daily activities in various groups.
The first wave of COVID-19 in Korea began at Sincheonji Church and occurred mostly in Daegu and Gyeongsangbuk-do Province. The second wave spread at rallies and religious facilities in the Seoul metropolitan area. The third wave, however, does not involve massive outbreaks in certain areas or groups, and has spread evenly to every corner of the nation. The silent spread of COVID-19 has permeated daily life in every corner of the country. What can be done to stop it?
[Soundbite]
Choi Young-il (Social critic): Let’s discuss this further with Professor Lee Jae-gap.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Hello.
[Soundbite]
Choi Young-il (Social critic): In your opinion, what is the leading cause of the third wave of COVID-19?
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): COVID-19 is relentlessly spreading through local communities. The biggest factor is the season. As the weather gets cold, people spend more time indoors. This will likely contribute to continued large-scale spread.
[Soundbite]
Choi Young-il (Social critic): We’re standing at a critical juncture. There's been many days with over 1,000 new cases. We’re seeing hundreds of cases daily, and they need to be hospitalized. Some of them have serious symptoms and the death toll has been rising recently. Shortage of hospital beds is one of the most concerning issue these days.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): As of December 17, about 40 ICU beds were available nationwide. Quarantine centers and infectious disease hospitals are around 70 percent full. The government is trying to secure 300 ICUs by early 2021 and provide 7,000-10,000 more hospital beds. ICU patients are the greatest concern. Hospitals could run out of ICU beds within a couple of weeks. We must secure more ICU beds at general hospitals, university medical centers or private hospitals as soon as possible.
[Soundbite]
Choi Young-il (Social critic): Let’s hear from Professor Ki Mo-ran. Hello, Professor. Concerns grow over the shortage of hospital beds in the capital area. What measures has the government devised to address the situation?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): So far, COVID-19 patients have been treated at public hospitals. But it’s not enough. We are asking private hospitals to help. Some hospitals have agreed to treat COVID-19 patients. But we need more such cooperation to solve bed shortages.
[Soundbite]
Choi Young-il (Social critic): The outbreak is becoming very protracted. It’s been almost a year now. The primary concern is health workers’ burnout and the shortage of nurses. Professor Lee, you probably know better than anyone what the health workers are going through.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): It’s a tough time for medical workers. But they continue doing their job because patients need them. I am worried they will be pushed to their limits if there are too many patients. All medical workers are urging the public to follow social distancing rules to reduce the number of patients so that nobody is rejected hospital treatment and all ICU patients can receive help.
This public hospital in Incheon has eleven ICU beds, but only four of them can be operated.
[Soundbite]
Cho Seung-yeon (Director of Incheon Medical Center): To treat seven more ICU patients, we need five doctors and 15-20 nurses.
Medical workers taking care of critically ill COVID-19 patients must wear Level D hazmat suits and work around the clock in shifts. This means more nurses are required than for other ICU patients.
[Soundbite]
Choi Young-il (Social critic): The question is how medical workers can be rewarded and encouraged to do their job. Of course, financial reward is an option. But the most fundamental solution is expanding the number of health workers. What do you think, Professor?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): Financial reward is one of the ways to do it. What needs to be done eventually is reducing workload. Nurses and medical technologists should be allowed to perform doctors’ duties. The number of medical personnel should be increased. If social distancing measures are raised and many facilities close down, the social cost will be enormous. It’d be more efficient to hire and train more health workers so that more patients can receive treatment.
[Soundbite]
Choi Young-il (Social critic): The protracted pandemic has resulted in shortage of beds
and health workers’ burnout. Many experts say the ultimate game changer will be a vaccine. U.S. President Donald Trump recently issued an executive order to administer vaccines to the American public first. Many in Korea worry that the country’s efforts to buy and provide vaccines could be stymied. What’s your take on this?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It’s been almost a year since the COVID-19 pandemic began. Instead of cooperating, each country only cares about its people. The pandemic will not be over if only one country is vaccinated. I hope the U.S. will understand this soon. I don’t think we need to worry about securing vaccines in Korea. First of all, the infection rate in Korea is quite stable compared to the U.S. or the U.K. Some say we must follow Germany and implement a lockdown. Germany has 20 times more cases than Korea. It's a different situation. Once a vaccine is brought to the country, it will be first administered to the residents and workers of high-risk, long-term care facilities. After inoculating about 10 million people, medical workers will be able to treat coronavirus patients with less worry.
[Soundbite]
Choi Young-il (Social critic): Many people in Korea want to know when they will be inoculated. The government at first said vaccination would start in the second quarter or second half of 2021. But lately it moved it up to February-March. Can vaccination begin even earlier than that?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): It would be difficult. There must be companies that have already applied or emergency use authorization. t takes more than a month to deliberate vaccine safety.
[Soundbite]
Choi Young-il (Social critic): The development of COVID-19 treatments is also a major concern, because infected patients need to be treated as soon as possible. Korean companies such as Celltrion and Green Cross are also developing coronavirus treatments. When can they be utilized to treat patients?
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The antibody treatment developed by Celltrion can be utilized soon. The results of Phase 2 clinical trials are to be released soon. Then the company can apply for emergency use authorization. If the treatment is approved before Phase 3 trials, it will be utilized within this year. Clinical trials are conducted on patients to prevent further aggravation of symptoms. Once safety is verified, treatments can be approved for immediate use even if their efficacy is somewhat low.
[Soundbite]
Choi Young-il (Social critic): COVID-19 is a new virus different from anything we've experienced before. Nobody knows if it can be eradicated. Then how should we change our lives to live with this virus?
[Soundbite]
Jung Eun-kyeong (Director of KDCA): Ironically, the only way to join hands in the era of COVID-19 is to stay apart and maintain a safe distance. Coronavirus is invisible, but it is spread continuously and survives when people meet. We can stop the spread if we avoid contact with others.
[Soundbite]
Ki Mo-ran (Head of COVID-19 task force Korean Society for Preventive Medicine): The COVID-19 pandemic has changed the world as we know it. It is a crisis. But to some, it’s an opportunity. In times like these, we must lend a helping hand to those in need so that we can beat the virus together.
[Soundbite]
Lee Jae-gap (Department of Infectious Disease, Hallym University): Viruses, bacteria and microorganisms will continue to threaten humans in the future. During outbreaks of infectious diseases, the most vulnerable groups in our society are most adversely affected by it. We need to find ways to better protect them. COVID-19 has profoundly changed our society. We can make our country safe and become the most successful nation in fighting COVID-19 five to ten years from now if we adapt to these changes and work together.
[Soundbite]
Choi Young-il (Social critic): We can beat COVID-19 only through social distancing, wearing masks and following precautions thoroughly. There are no shortcuts. It’s important to keep in mind that each individual’s ill-advised actions can put an entire community at risk.
After a long fight against COVID-19, Korea’s quarantine efforts seem to be losing ground. However this pandemic has taught us that we can beat this virus only if the public, medical workers and the government join hands under the common goal.
이 기사가 좋으셨다면
-
좋아요
0
-
응원해요
0
-
후속 원해요
0










![[속보] 경남 김해에 시간당 70mm 이상 집중호우, <br>침수 주의](/data/news/2025/07/13/20250713_NQ5jSr.jpg)
![[단독] 위성락 실장 “전작권 협상 카드 아냐”…차관 인선 발표](/data/layer/904/2025/07/20250713_krfuHu.jpg)


이 기사에 대한 의견을 남겨주세요.